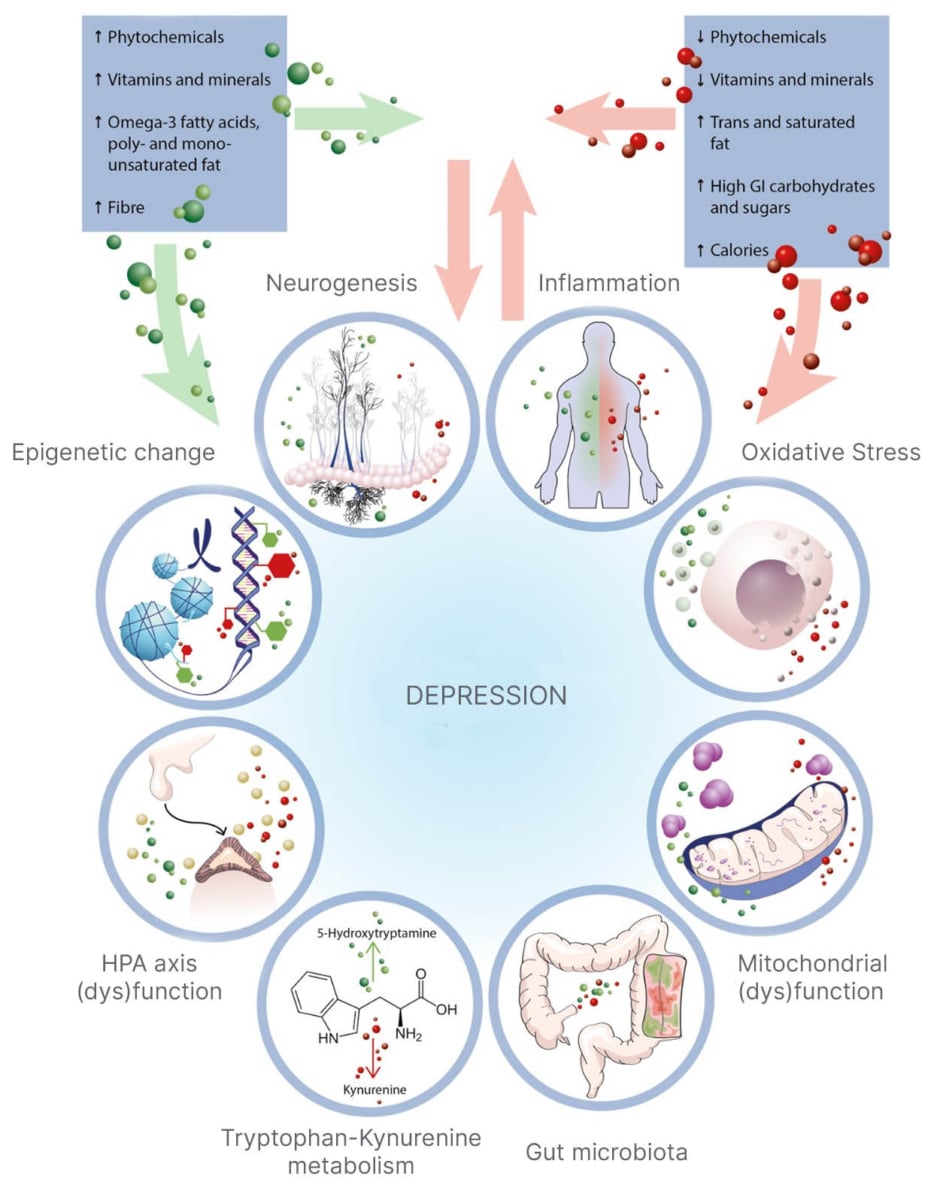
It is becoming increasingly clear that what we eat plays a critical role in brain health. Diet influences oxidative stress, neuroinflammation, mitochondrial function, and even the composition of our gut microbiota. These biological processes directly impact neurotransmitter balance, mood regulation, and cognitive performance.
Mental health disorders are now among the leading causes of disability worldwide. According to WHO over 1 billion people globally live with a mental health condition approximately 1 in 7 individuals. Since 2020, rates of anxiety and depression have increased by roughly 25% worldwide, marking one of the most significant global surges in mental health challenges in modern history.
While medications, supplements, psychotherapy, and exercise remain essential pillars of care, nutrition is an often underexplored yet powerful therapeutic tool. The field of nutritional psychiatry continues to demonstrate that dietary quality significantly influences mental health outcomes.
Gut-Brain Axis
The gut–brain axis is a complex bidirectional communication network connecting the gastrointestinal system and the central nervous system. This communication occurs through:
-
Neural pathways (particularly the vagus nerve)
-
Immune signaling
-
Endocrine (hormonal) pathways
-
Microbial metabolites

- Photo retrieved from: Chen et al., 2025
The microbiota–gut–brain axis highlights the critical role of gut microbes in influencing:
-
Neural development
-
Neurotransmitter production
-
Stress response regulation
-
Behavioural patterns
Alterations in gut microbiota (dysbiosis) may contribute to the development or progression of neurological, neuropsychiatric, and neurodevelopmental disorders. Increased intestinal permeability (“leaky gut”), systemic inflammation, and neuroinflammation are emerging mechanisms linking diet to mental health conditions (Chen et al., 2025).
NOVA Classification System

The NOVA classification system, developed by Monteiro and colleagues, categorizes foods according to their degree of industrial processing into four groups:
-
Unprocessed or minimally processed foods
-
Processed culinary ingredients
-
Processed foods
-
Ultra-processed foods (UPFs)
Ultra-processed foods are industrial formulations made primarily from refined substances and additives, containing little to no whole foods. They often include:
-
Artificial sweeteners
-
Emulsifiers
-
Preservatives
-
Flavor enhancers
-
Refined sugars
-
Industrial seed oils
-
High sodium content
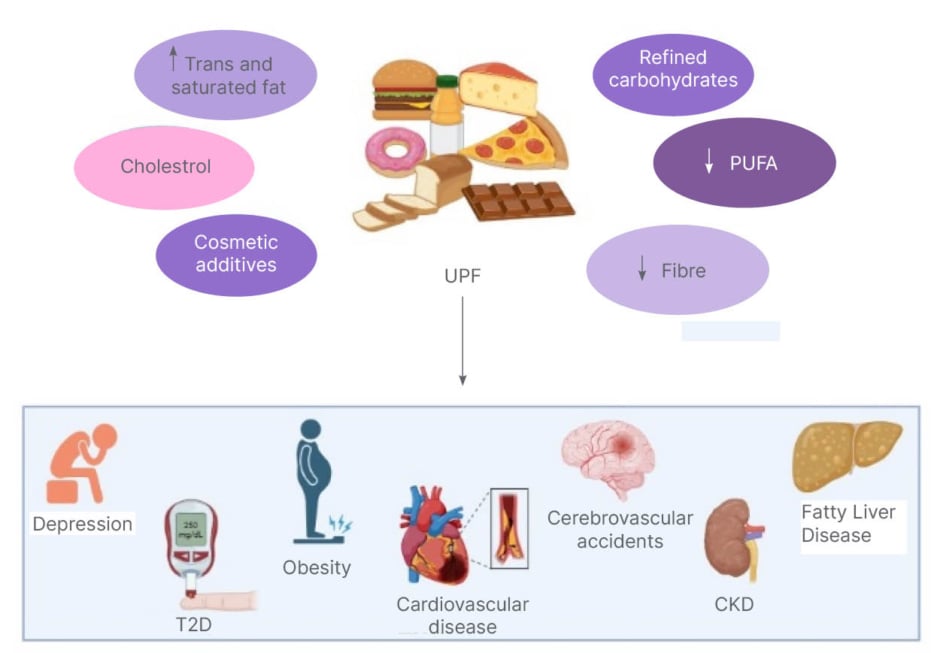
UPFs are engineered to be hyper-palatable and shelf-stable. Their increased consumption globally has been associated with:
-
Internalizing symptoms
-
Anxiety
-
Depression
-
Insulin resistance
-
Cognitive decline
-
Neuroinflammation
Research suggests individuals with higher UPF intake have a 20–50% greater risk of developing depressive symptoms (Karim et al., 2025).
-
Photo Derived from Karim et al., 2025
Depression and Ultra-Processed Food
Depression
According to the DSM-5, Major Depressive Disorder requires at least two weeks of persistent symptoms, including depressed mood or loss of interest/pleasure, along with additional symptoms such as:
-
Changes in appetite or weight
-
Sleep disturbances
-
Fatigue
-
Psychomotor agitation or slowing
-
Feelings of worthlessness or guilt
-
Impaired concentration
-
Suicidal ideation
Nutritional Risk Factors
-
Ultra-processed foods
-
Refined carbohydrates
-
Excess dietary sugar
-
Industrial seed oils
-
Excess caffeine
-
Alcohol
- Photo Derived from Karim et al., 2025
A recent systematic review found that higher consumption of ultra-processed foods is associated with increased risk of depression, particularly with high intake of artificial sweeteners and processed beverages (Samuthpongtorn et al., 2023).
Potential mechanisms include:
-
Increased inflammatory mediators
-
Oxidative stress
-
Neuroinflammation
-
Altered neurotrophic growth factor expression
-
Impaired glucose metabolism
-
Disrupted purinergic signaling
High added sugar intake has been significantly associated with increased risk of depression. European cohort studies further suggest that diets high in added sugars and high glycemic index foods, coupled with low nutrient density, increase the risk of anxiety and depressive disorders (Ulger et al., 2025).
Frequent UPF consumption has also been associated with reduced hippocampal volume, a structure critical for mood regulation and neuroplasticity (Wang et al., 2024).
Anxiety Disorders
Anxiety disorders are the most prevalent psychiatric conditions, affecting approximately 30% of adults at some point in their lives.
Dietary Contributors
High sugar intake has been linked to:
-
Negative neuroplastic changes
-
Increased impulsivity
-
Dysregulated dopamine pathways
-
Neuroinflammatory processes (elevated IL-6, TNF-α, leptin, iNOS)
Chronic sugar consumption may enhance oxidative stress and inflammation in brain regions involved in anxiety regulation (Norwitz & Naidoo et al., 2021).
Large population-based data (n = 140,728) demonstrate that frequent fried food consumption particularly fried potatoes is associated with:
-
12% higher risk of anxiety
-
7% higher risk of depression
Acrylamide exposure from fried foods may dysregulated lipid metabolism and increase neuroinflammation (Wang et al., 2023).
Nutrition Strategies for Anxiety
-
Reduce processed sugar
-
Minimize fried foods
-
Lower caffeine intake
-
Reduce inflammatory vegetable oils high in omega-6 linoleic acid
-
Consider gluten sensitivity in susceptible individuals
Obsessive–Compulsive Disorder (OCD)
Obsessions
-
Recurrent, intrusive, unwanted thoughts, images, or urges
-
Often distressing or anxiety-provoking
-
Common themes include contamination, harm, symmetry, morality, or doubt
-
Examples:
-
-
Fear of germs or contamination
-
Repeated doubts (e.g., “Did I lock the door?”)
-
Intrusive violent or taboo thoughts
-
Compulsions
-
Repetitive behaviors or mental acts performed to reduce anxiety caused by obsessions
-
The behaviors are often excessive or not logically connected to the fear
-
Examples:
-
-
Excessive hand washing
-
Checking locks repeatedly
-
Counting, praying, or repeating phrases silently
-
Emerging research suggests that abnormal glutamatergic neurotransmission plays a significant role in OCD pathophysiology. Elevated cerebrospinal glutamate levels have been observed in patients with OCD.
Potential Nutritional Influences
Glutamate-rich foods include:
-
Aged cheeses
-
Soy sauce
-
Processed foods with added MSG
-
Cured meats
-
Tomatoes
-
Mushrooms
While dietary glutamate research remains underdeveloped, modulation of glutamatergic activity through diet represents a promising future area of exploration.
Supportive Nutrients
-
Vitamin E (often found lower in OCD patients)
-
Vitamin C
-
Glutathione-supportive foods
-
Glycine (modulates NMDA receptors)
-
Tryptophan-rich protein foods
Vitamin E–rich foods include:
-
Almonds
-
Sunflower seeds
-
Spinach
-
Kale
-
Wheat germ oil
These antioxidants may help reduce oxidative stress markers such as malondialdehyde (MDA), which has been found elevated in OCD populations (Sarkar & Sarkar et al., 2024).
Bipolar Disorder
Bipolar disorder is a mood disorder characterized by alternating episodes of:
Mania or Hypomania
- Periods of elevated or irritable mood with increased energy.
- Symptoms may include:
-
-
Decreased need for sleep
-
Racing thoughts
-
Increased talkativeness
-
Impulsivity or risky behavior
-
Inflated self-esteem
-
In severe mania, psychosis may occur.
Depression
- Episodes of low mood similar to major depressive disorder:
-
Persistent sadness
-
Fatigue
-
Loss of interest
-
Changes in appetite or sleep
-
Difficulty concentrating
-
Bipolar disorder is categorized into types:
-
Bipolar I – At least one full manic episode
-
Bipolar II – Hypomania and major depressive episodes
Dietary patterns influence inflammatory and oxidative pathways implicated in bipolar disorder (BD).
Dietary Risk Factors
-
Refined sugars
-
High glycemic load foods
-
Saturated fats
-
Ultra-processed foods
-
Excess sodium
-
Excess caffeine
Supportive Nutrients
-
Omega-3 polyunsaturated fatty acids (PUFAs)
-
Seafood
-
Folate
-
Zinc
-
Polyphenol-rich foods
-
Mediterranean-style dietary patterns
Omega-3 fatty acids are particularly important for:
-
Neuronal membrane fluidity
-
Serotonin signaling
-
Anti-inflammatory modulation
-
Protection against oxidative damage
Dietary patterns high in saturated fat and refined sugars promote systemic inflammation, oxidative stress, mitochondrial dysfunction, and impaired neuroplasticity mechanisms strongly implicated in mood instability.
Nutritional psychology highlights a foundational truth: the brain requires high-quality fuel to function optimally.
Inflammatory diets rich in ultra-processed foods, refined sugars, and industrial oils may:
-
Disrupt gut microbiota
-
Increase systemic inflammation
-
Impair mitochondrial energy production
-
Alter neurotransmitter balance
-
Reduce neuroplasticity
Conversely, whole-food, nutrient-dense, anti-inflammatory dietary patterns may serve as powerful adjunctive tools in mental health care (Gabriel et al., 2023).
For clinicians practicing integrative and naturopathic medicine, nutrition represents a low-risk, foundational intervention that can significantly complement conventional psychiatric treatments.
Final Thoughts
Nutritional psychology highlights a foundational truth: the brain requires high-quality fuel to function optimally.
Inflammatory diets rich in ultra-processed foods, refined sugars, and industrial oils may:
-
Disrupt gut microbiota
-
Increase systemic inflammation
-
Impair mitochondrial energy production
-
Alter neurotransmitter balance
-
Reduce neuroplasticity
Conversely, whole-food, nutrient-dense, anti-inflammatory dietary patterns may serve as powerful adjunctive tools in mental health care.
For clinicians practicing integrative and naturopathic medicine, nutrition represents a low-risk, foundational intervention that can significantly complement conventional psychiatric treatments.
References:
Chen, C., Wang, G., Li, D., et al. (2025). Microbiota–gut–brain axis in neurodegenerative diseases: Molecular mechanisms and therapeutic targets. Molecular Biomedicine, 6, 64. https://doi.org/10.1186/s43556-025-00307-1
Gabriel, F. C., Oliveira, M., Bruna De M Martella, Berk, M., Brietzke, E., Jacka, F. N., & Lafer, B. (2023). Nutrition and bipolar disorder: a systematic review. Nutritional neuroscience, 26(7), 637–651. https://doi.org/10.1080/1028415X.2022.2077031
Karim, S., Alam, A. S., & Syed, A. (2025). Association between ultra processed food consumption and risk of developing depression in adults: A systematic review. EMJ Gastroenterology, 14(1), 64–74. https://doi.org/10.33590/emjgastroenterol/IVVG9805
Wang, X., Wong, A. C. W., Sheng, Z., Wong, S. Y.-S., & Yang, X. (2024). The relationship between dietary sugar consumption and anxiety disorders: A systematic review. Nutrition Bulletin. Advance online publication. https://doi.org/10.1111/nbu.12702
Samuthpongtorn, C., Nguyen, L. H., Okereke, O. I., Wang, D. D., Song, M., Chan, A. T., & Mehta, R. S. (2023). Consumption of Ultraprocessed Food and Risk of Depression. JAMA network open, 6(9), e2334770. https://doi.org/10.1001/jamanetworkopen.2023.34770
Sarkar, S., & Sarkar, S. (2024, April). Nutritional and dietary role in neuropsychiatric disorders: Depression and obsessive compulsive disorder (OCD).
Ülger, T. G., Sürücü, B., Menekşe, A. E., Çakmak, Y., Fidan, Ş., & İncekara, B. (2025). The effect of dietary carbohydrate quality on depression and anxiety levels in adolescents. Frontiers in nutrition, 12, 1689004. https://doi.org/10.3389/fnut.2025.1689004
Wang, A., Wan, X., Zhuang, P., Jia, W., Ao, Y., Liu, X., Tian, Y., Zhu, L., Huang, Y., Yao, J., Wang, B., Wu, Y., Xu, Z., Wang, J., Yao, W., Jiao, J., & Zhang, Y. (2023). High fried food consumption impacts anxiety and depression due to lipid metabolism disturbance and neuroinflammation. Proceedings of the National Academy of Sciences of the United States of America, 120(18), e2221097120. https://doi.org/10.1073/pnas.2221097120
Wang, X., Wong, A. C. W., Sheng, Z., Wong, S. Y.-S., & Yang, X. (2024). The relationship between dietary sugar consumption and anxiety disorders: A systematic review. Nutrition Bulletin. Advance online publication. https://doi.org/10.1111/nbu.12702
About the author:

Hi, I’m Abinaa, a fourth-year naturopathic medical student at the Canadian College of Naturopathic Medicine with a deep-rooted passion for natural healing, inspired by my South Asian upbringing. Through this blog, I hope to share my journey, explore topics in holistic health and wellness, and offer simple, thoughtful insights that support a more balanced and mindful way of living.




